Introduction:
Sickle cell disease (SCD) exerts a significant morbidity and mortality burden worldwide, with 300,000 infants being diagnosed with SCD annually. The term sickle cell crisis (SCC) encompasses several acute conditions under its umbrella, namely vaso-occlusive crisis, aplastic crisis, splenic sequestration crisis, dactylitis, and acute chest syndrome. SCC has been established to be a known cause of readmissions across the year with studies showing 17% of the population returning two to three times annually. This has resulted in a high mean length of stay for this diagnosis (5.3 days) in comparison to an index hospitalization (4.9 days), with a mean cost of $8485 per admission. Readmissions owing to SCC have relayed a significant burden of 95,445 hospitalization days and a total charge of $609 million in the US. Despite the high morbidity and financial burden it imposes, limited studies have been performed studying the risk factors for readmissions in these patients. Despite the establishment of a framework of recommendations and guidelines, there appears to be a high incidence of readmissions and discrepancies in adherence to evidence based recommendations. We performed a retrospective study to evaluate the risk factors for patients hospitalized in three community hospitals between October 2021 and August 2022.
Methods:
The admissions database of a community health system across three hospitals was scanned for admissions with SCC between the time period October 2021 and August 2022. ICD9 and ICD-10 codes of SCC were used. 50 patients found with the admitting diagnosis code of SCC and 103 encounters were included. After excluding patients who left against medical advice before initiation of treatment, those with the wrong diagnosis and incomplete documentation, a cohort of 47 patients with 100 encounters was attained. Patient charts were reviewed and demographic variables such as age, gender and race were studied. Readmissions and the length of stay were assessed for risk factors with the help of a chi square test. Risk factors assessed included use of pain medications (opioids with non-steroid anti-inflammatory medications versus monotherapy), use of IV Fluid Boluses, placement of Hematology consult, having an established primary care physician and the use of hydroxyurea as a home medication.
Results:
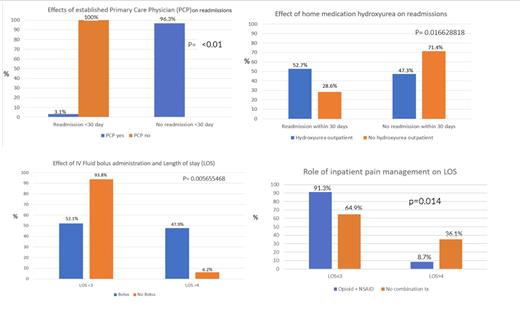
87% of the patient population was African American with equal gender distribution (Males 51%; Females 49%). 59% of the patient population lay in the age group of 18-35. 49% of the patient population was noted to have readmissions within the time frame studied with 29% of the patient population having a length of stay of more than 3 days. 100% of the patients without an established primary care physician (PCP) were noted to have readmissions in comparison to 3.6% of the patients with an established PCP (p< 0.01). Length of stay was less than 3 days for 91.3% of the patients treated with the combination of opioids and NSAID's for pain in comparison to 64.9% of the patients that were not treated with this combination (p= 0.014). It was noted however, that 37% of the population was on hydroxyurea outpatient and 44% of the cases had involved hematology for the inpatient management of these patients. IV Fluid boluses and their association with length of stays in our patient population was unequivocal. 52.7% of the patients on hydroxyurea had readmissions within 30 days as opposed to 28.6% of the patients not on the drug. This was likely explained by non-compliance to the medication. No deaths were reported in this patient cohort.
Conclusion:
Several risk factors for readmissions in SCC patients exist in the community setting. Our findings reported that lack of close outpatient follow up is associated with higher readmission rates. In addition, we also observed that the type of medical pain management (combination vs monotherapy) played a role in length of stay with combination therapy being linked to shorter hospitalization stay. Integrated education for various medicine specialties regarding management guidelines should be instituted. In addition, maximum utilization of social work and case management for ensuring close follow ups for this patient population may further mitigate readmissions of SCC patients in the community setting.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal